
30 April 2019
Innovation in healthcare: Are we taking it too far?
Isabelle Mansour is a Health Planner in TSA’s Sydney office. Her Bachelor of Nursing Sciences and Masters in Health Services Management, combined with her health experience give her an expert understanding of health facility planning.
Isabelle is currently working on the $534 million Tweed Hospital Project for Health Infrastructure NSW.
I recently attended the Australian Healthcare Week (AHW) at the International Convention Centre, Darling Harbour. AHW is the largest healthcare event in Australia and the annual meeting place for the healthcare community to connect, network and explore the future of the design, delivery and operation of Australia’s healthcare system. The central theme for this year was future-proofing our health facilities and workforce to serve more complex patients in a dynamic digital environment.
As part of TSA Health Planning team, I am closely involved in the project user groups consultation process for the planning of hospital development projects, where this can be directly implemented. I find innovation in healthcare a topic that is equally capturing the interest of healthcare professionals, patients and carers. Hospitals are future-proofing their designs to integrate digital innovation in their service models and deliver better and more affordable patient-centred care. Meanwhile, patients are embracing the introduction of technology in their health journey and being self-empowered to co-manage their own recovery and treatment alongside the clinician.
During the expo, I was particularly drawn to the sessions focusing on the future direction for healthcare to embrace digital disruption, drive innovation and deliver better health outcomes.
Dr. Anjail Jalprakash, a research fellow from the Queensland University of Technology, Medical and Healthcare Robotics Group talked through the evolution of robotics vision. She presented a picture of a factory where multiple robots were involved in the production process, with minimal human intervention. In contrast, the speaker showed a photo from an operating theatre, involving a number of clinicians, performing a surgical procedure on a patient.
The aim of this session was to highlight that over the past decade, medicine has been slower to adopt technology compared to other industries. Despite the enormous interest in big-data analytics, integration of patient information, telehealth and artificial intelligence tools, the concept of factory-like hospitals has been slower to be accepted and incorporated in patient care.
 |  |
|---|
Manufacturing process lead by robots vs. Surgical procedure lead by clinicians.
One of the sessions I attended was presented by the Director of Critical Care Centre, Memorial Sloan Kettering Cancer Centre (MSKCC) in New York. He explained the MSKCC is leading the way in designing the futuristic Intensive Care Units (ICUs) and adapting technologies to improve customer experience and the quality of critical care delivery. Their vision for ICUs for the year 2050 includes the design of “biosphere capsules” which will monitor the patients’ environment using advanced sensors, visors to transform and communicate the patient’s thoughts, holographic doctors to provide remote care and other technological innovations which will transform the way medicine is practiced.
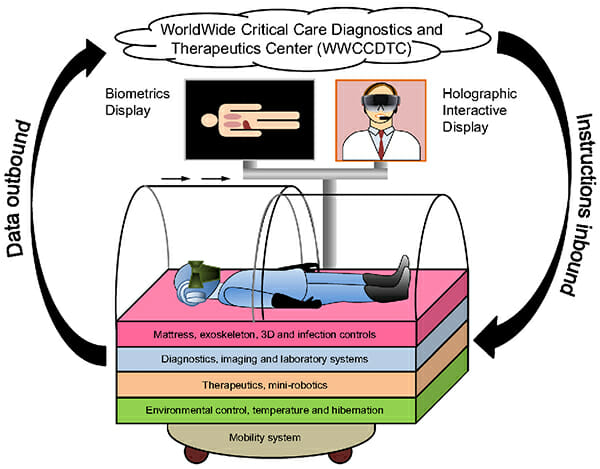
Biosphere capsule and other technological innovations – Vision for the 2050 ICUs
There is little doubt that the implementation of such technological innovation will have significant benefits including making it easier for health professionals to monitor patients, reduce the need for excessive wiring of patients and freeing up clinicians in hospitals to carry out more complex cases. I challenged the speaker to consider consulting with patients during the design process as the capsule looked like a giant fishbowl and some patients may not prefer this over being wired in a bed.
Another captivating topic was the Virtual Reality Health Service. It consists of delivering comprehensive clinical care to patients regardless of where they live and what ground systems are available. During the session we heard about how this has already been implemented in NSW e.g. Western NSW Local Health District use telehealth to provide specialist advice to remote areas. The Mid North Coast Local Health District has introduced “Telestroke”, a project that is improving outcomes for patients who present to Port Macquarie and Coffs Harbour Hospitals with stroke symptoms. Telestroke is allowing to bridge distances and deliver world-class stroke assessment, treatment and management, irrespective of patients’ location. This is important for rural communities as patients often travel long distances to reach the nearest hospital and that hospital may not have the specialists to treat and manage these patients and have to transfer them to other hospitals.
There are multiple advantages of technology in healthcare and this cannot be overlooked, including:
- robots performing surgery are claimed to reduce the risk of human error;
- automated pharmaceutical dispensing machine is declared to limit medication administration errors and promote efficiency;
- telehealth fosters equity of access to advanced and timely medical care;
- digitalised health records enhance patient care through improving access to big data, etc.
However, are we ready to fully rely on machines and let the virtual world completely take over from a human in delivering patient care? Are we overlooking the importance of the human touch in the patients’ recovery and healing process, both physically and emotionally? Before going too far in designing future healthcare innovations and thinking of future-proofing our healthcare facilities to accommodate them, are we truly involving the end-user (patients) in these decisions? Or are we just assuming that if we simply design an innovative hospital or service the “right way” and in compliance with relevant guidelines and policies, patients will undoubtfully embrace it?
Despite the challenges, I believe that the benefits of technology far outweighing the disadvantages. Moving forward, the key is to find the correct balance so that the efficiencies and precision of technology coupled with the human touch are used to provide optimum patient and experiences.


